About sepsis and systemic inflammation
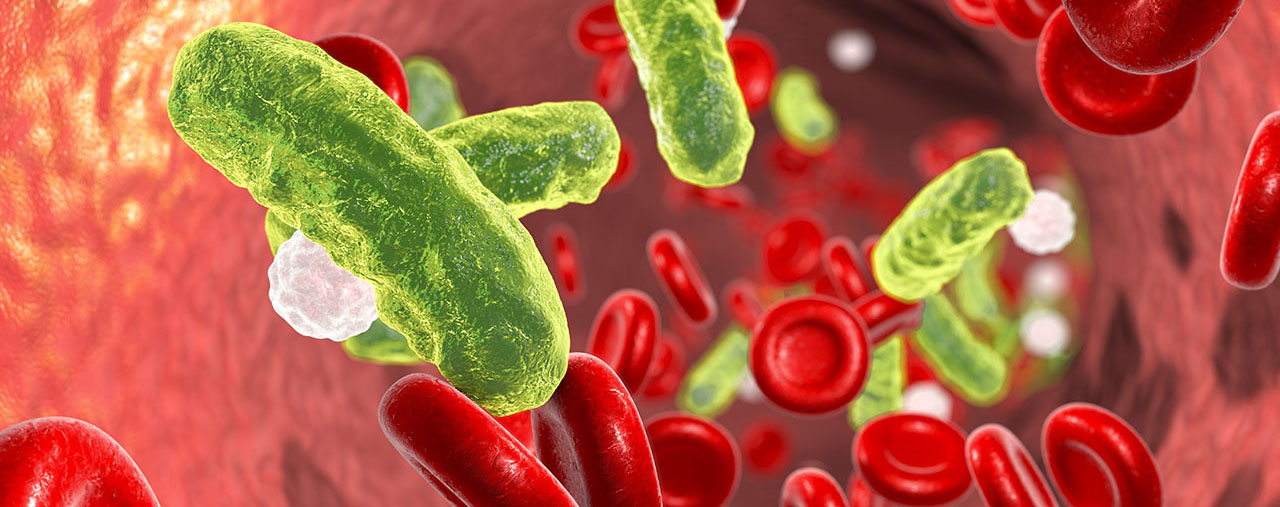
Severe systemic inflammation (also known as systemic inflammatory response syndrome, SIRS) is a feared complication of severe medical conditions such as sepsis, trauma, and major surgery. It is characterized by an uncontrolled systemic inflammatory response that can progress into shock and multi-organ failure. Septic shock, the most severe form of sepsis, is a leading cause of death in intensive care units worldwide, with mortality rates typically exceeding 30%1.
Vascular hyper-permeability caused by inflammatory activation, may cause significant endothelial damage, plasma leakage and excessive edema formation. The pulmonary circulation is particularly vulnerable, leading to respiratory distress, and in time more advanced multi-organ damage ensues. Neutrophil granulocytes, releasing an array of cationic proteins exhibiting permeability–increasing properties, are critically involved in the capillary-alveolar barrier breakdown.
Sepsis, a common form of severe systemic inflammation, is one of the costliest conditions to treat in the hospital care setting2. In the US in-patient care cost a total of $22 billion in 2019, a figure that has increased from the $17 billion in 2012. Additional data from the UK estimates the direct cost of treating patients with sepsis in intensive care was £0.8 billion in 2017, while the broader costs to society, including indirect costs, amounted to £10 billion (YHEC The Cost of Sepsis Care, the UK Final Report 2017).
There is currently no pharmaceutical product available that can be specifically used to treat patients with sepsis or other forms of uncontrolled systemic inflammation. The current standard of care for hospitalized patients relies on aggressive fluid therapy, vasopressors, oxygen, corticoid steroids, and mechanical ventilation, in addition to antibiotics.
Preclinical data both in cells and in mouse in-vivo models show the potential for sevuparin in protecting the blood vessels primarily of the lung vasculature by affecting white blood cells and their actions, which is supported as well by clinical findings in healthy volunteers during induced systemic inflammation (LPS-challenge).